Author: Mark Akinware

In a concerning development for global healthcare, scientists have uncovered how the superbug Clostridioides difficile (C. diff) rapidly evolves resistance to one of the most critical antibiotics used in treatment—vancomycin. This discovery, made by researchers from the University of Sheffield and the University of Manchester, underscores the urgent need for vigilant monitoring and proactive measures to combat antimicrobial resistance (AMR).
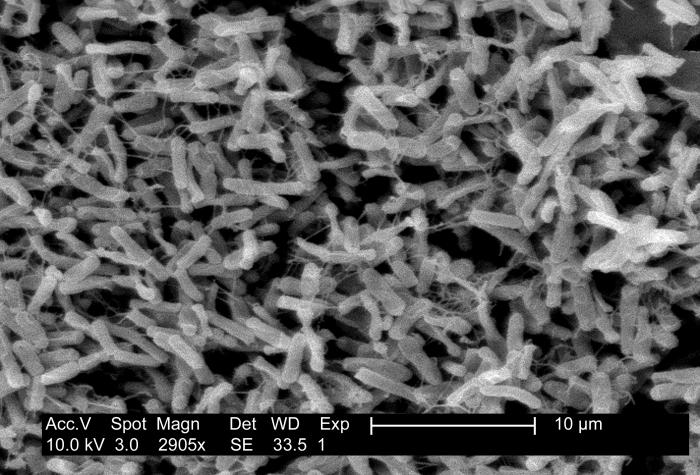
Clostridium difficile bacteria, Source: CDC.gov
The Alarming Evolution of Vancomycin Resistance:
Clostridioides difficile is a bacterium often associated with antibiotic use, leading to severe infections in vulnerable patients. In the UK alone, C. diff is responsible for approximately 2,000 deaths annually. The recent study has revealed that C. diff can develop resistance to vancomycin at an alarming rate—within just two months, the bacteria can tolerate antibiotic concentrations 32 times higher than what is normally effective. This rapid evolution of resistance poses a significant threat to public health.
Vancomycin is a frontline treatment for C. diff infections, but its effectiveness is now at risk. Despite the critical role vancomycin plays in healthcare, routine monitoring for resistance is not yet standard practice in clinical settings. This oversight could allow resistance to spread unnoticed, potentially leading to a scenario where vancomycin is no longer a viable treatment option.
The Consequences of Vancomycin Resistance:
The implications of this resistance are profound. Currently, antibiotics like vancomycin can damage beneficial gut bacteria, leading to a high rate of reinfection. Up to 30% of patients treated with vancomycin experience a second infection within weeks, and the likelihood of further relapses increases with each occurrence. If vancomycin resistance becomes widespread, the ability to effectively treat C. diff infections could be severely compromised.
Dr. Jessica Buddle, a PhD candidate at the University of Sheffield and the lead author of the study, emphasises the importance of monitoring this resistance:
“Unchecked resistance could contribute to the large number of patients who have a relapsing infection after successful treatment with vancomycin. More research is essential to inform healthcare policy and determine if vancomycin remains the best treatment option.”
The Role of Fitness Costs in Resistance Management:
While the emergence of vancomycin resistance in C. diff is alarming, there is a silver lining. The resistant strains identified in the study exhibited reduced overall fitness, which may limit their ability to cause widespread clinical harm. Specifically, these strains often had defects in sporulation—a process crucial for C. diff to transmit from person to person and survive on hospital surfaces.
This reduced fitness could be exploited to develop new treatments. According to Professor Michael Brockhurst from The University of Manchester:
“Such fitness costs are a pathogen’s Achilles’ heel and could potentially be exploited to devise new treatments that reduce the burden of drug-resistant infections in the future.”
The Global Impact of Antimicrobial Resistance:
The rapid development of vancomycin resistance in C. diff is part of a broader, global challenge posed by antimicrobial resistance (AMR). The World Health Organization (WHO) has identified AMR as one of the top public health threats of our time, with bacterial AMR directly responsible for an estimated 1.27 million deaths globally in 2019 alone.
Understanding the genetic mutations that drive resistance, as well as the associated fitness costs, is crucial for developing strategies to manage and mitigate the impact of AMR. The ongoing work by the research teams aims to simulate resistance development within the complex environment of the human gut and to collaborate with epidemiologists to identify resistance signatures in hospitals.
Looking Ahead: The Need for Vigilant Surveillance:
As the fight against AMR intensifies, the findings from this study highlight the urgent need for enhanced surveillance of antibiotic resistance in healthcare settings. By closely monitoring resistance patterns and understanding the trade-offs that resistant strains face, healthcare providers can better manage the risks associated with C. diff infections.
The stakes are high. If antibiotics like vancomycin are lost as effective treatments, common infections could once again become life-threatening. As researchers continue to explore new ways to combat resistance, the healthcare community must remain vigilant in its efforts to preserve the effectiveness of existing antibiotics.
For more detailed insights into this groundbreaking study, read the full paper published in the journal PLOS Biology here.

