Author: Ezinne Onwuekwe, Estelle Mbadiwe and Kenneth Egwu, – Mon. May 2 2023. 12:04 GMT +1

Background
The African continent has the highest mortality rate in the world, with a huge amount of the continent’s population affected by epidemics such as Malaria, HIV/AIDS, Polio, Ebola, Lassa fever, Money pox, and, Cholera. Just about 52% of the population, approximately 615 million people, have access to the healthcare they require[1]. Maternal and child mortality, non-communicable diseases, and neglected tropical diseases have also plagued the healthcare system in Africa for a long time. Some of these epidemic diseases are preventable, but there exists a weak healthcare system, stunted by limited and inaccurate information on disease prevalence, spread and surveillance. More so, in many African countries, this surveillance is not available due to a scarcity of competent health professionals, low healthcare spending, and a shortage of infrastructure to gather and monitor data.
Data is an essential tool for improving healthcare systems, as it facilitates planning and management of health services, monitoring performance on primary health care, as well as health systems strengthening for Universal Health Coverage. The performance of a health system is strongly related to the quality of produced health information. Quality health information (credible, coherent, up to date, etc.) allows the health system to be effective and efficient in terms of decision-making by the health managers for resource planning, monitoring and evaluation of actions undertaken for health, and epidemiological surveillance [2]. In the recent past, the application of data in the African healthcare system has become a crucial component in improving healthcare delivery in the continent and has become increasingly important as the continent grapples with healthcare issues and seeks to improve healthcare outcomes.
Challenges
The healthcare sector in Africa faces significant challenges with regard to data collection, management, and use. Despite efforts by African governments and international organizations to improve the collection and use of healthcare data in Africa, the continent still lags behind other regions. According to the World Health Organization (WHO), African countries have the least developed healthcare information systems globally. Only about 50% of African countries have a functional health information system, compared to 90% in the Americas and Europe [3]. Healthcare funding in Africa is generally low, and this affects the quality of healthcare services and the ability of healthcare facilities to collect and manage health data. In 2020, African countries spent about $8 to $129 per capita on health, which is low compared to high income countries that spent above $4,000 [4]. Insufficient investment in the health sector is a serious obstacle to improving health outcomes in Africa. Consequently, facilities are often poorly equipped with limited access to technology and adequate infrastructure such as computers, internet connectivity, and power supply, which makes it difficult to collect, store, and analyze healthcare data. Many of the available data in the African healthcare systems are often incomplete, inaccurate, or outdated. Only 2.77% of countries in the region have digital health ecosystems that are fully interoperable, indicating the need for the countries to set up consolidated architecture to address data security and interoperability issues. Despite the fact that 76% of countries have developed their digital strategy or plan, only 14.7% of countries have implemented digital health projects [5]. This makes it difficult for healthcare policymakers and practitioners to make informed decisions. Healthcare facilities are ill-equipped to collect and analyze health data; health data is still mostly collected manually, and health workers sometimes have to fill out forms, which are later sent to data centers for processing. This process is slow and inefficient and can result in incomplete data. Such weak data collection system affects the quality and reliability of health data. Furthermore, the fragmented nature of healthcare systems in many African countries makes it difficult to collect and integrate data from different sources. This has resulted in silos of data that are not easily accessible to policymakers and practitioners.
Additionally, a lack of consistency in the data collected exists, with many healthcare facilities reporting different data on the same indicators. A robust platform for analytic support and triangulation of available data is needed. This would reduce fragmentation and duplication while improving efficiency [6]. Furthermore, the continent faces a shortage of qualified personnel in data management and analysis, and this hinders the effective use of health data in healthcare planning, monitoring, and evaluation Africa has 2.3 healthcare workers per 1000 population, compared with the Americas, which have 24.8 healthcare workers per 1000 population. Africa has only 1.3% of the world’s health workers to care for the vast population that suffers 25% of the global disease burden[7].
Health Care Spending
Figure 1: Share of Out-of-Pocket Expenditure on Healthcare in 2019
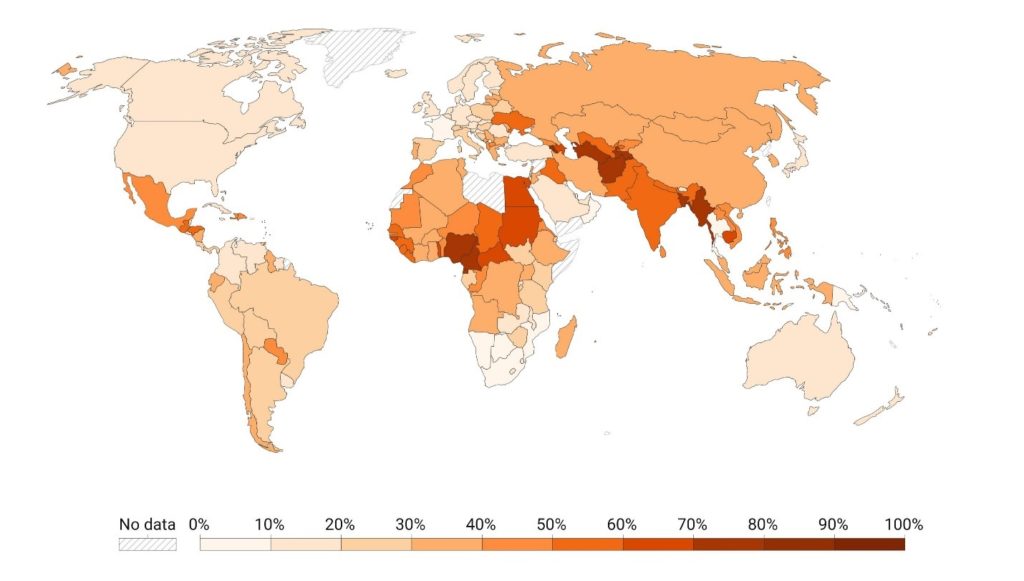
Source: World Health Organization (via Our World in Data
The 2001 Abuja Declaration; a commitment by the African Union member countries to increase the budget allocation on health by 15% has remained widely unattainable. Numerous African countries other than South Africa, Rwanda, Ethiopia, Gambia and Malawi, have failed to reach the target[8]. No country in West Africa has achieved the required 15% health priority index (Abuja declaration). However, the top three countries with the highest average health priority index in West Africa from 2010 to 2018 were Ghana (8.43%), Carbo Verde (8.29%), and Burkina Faso (7.60%), while Guinea (3.05%), Liberia (3.46%), and Guinea-Bissau (3.56%) had the lowest average health priority [9].
Figure 2: Total Health Expenditure as a Share of GDP, 2019
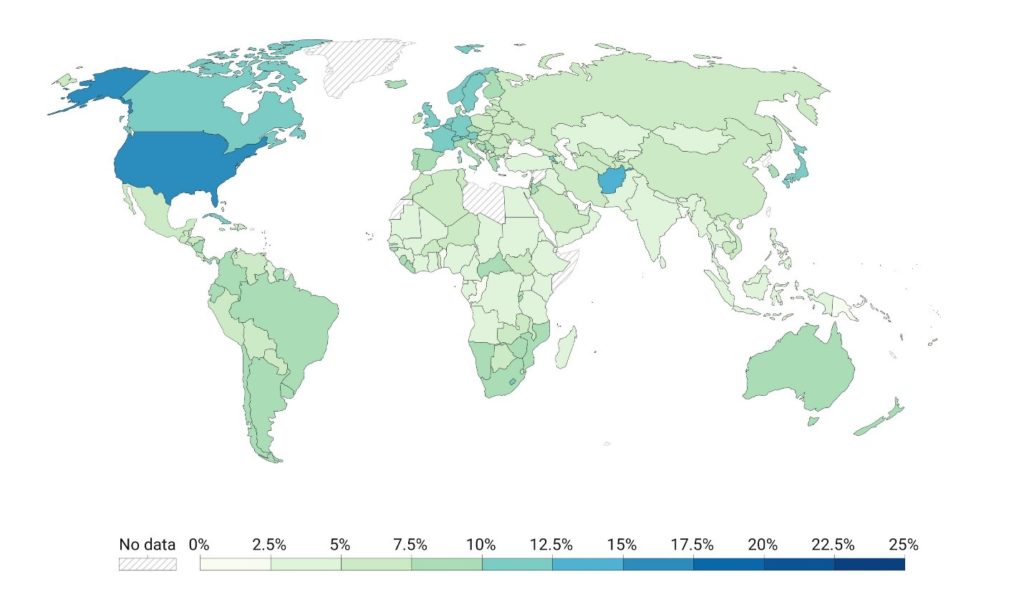
Source: WHO, Global Health Observatory (2022) (via Our World in Data)
With an average 5.3% of its GDP going towards health, the WHO African Region was rated fifth out of the six WHO regions in 2019 in terms of health financing. Between 2002 and 2011, the average expenditure in sub-Saharan Africa tripled from US$ 27 to US$ 90, after which it started to decline around 2014–2016 [10].
Some Progress Seen
Despite the challenges, some progress has been made in the collection and use of health data in the African healthcare system. For instance, the African Union launched the African Health Observatory in 2011, which aims to improve the availability, quality, and use of healthcare data in the continent. The observatory provides a platform for sharing healthcare data and information, and it also supports countries to develop their healthcare information systems. Recently in 2023, Africa Centres for Disease Control and Prevention (Africa CDC) launched its Digital Health Strategy, which aims to harness the power of digital technology to improve public health outcomes across the continent. Though the application of data in healthcare is still at a rudimentary level in Africa due to discussed bottlenecks, the rise in the use of the internet and mobile technologies in Africa have provided a platform for the generation of data, which are potentially useful in healthcare. In combatting infectious diseases, early detection, and surveillance are critical and healthcare administrators in Africa have harnessed the use of data in electronic surveillance to detect outbreaks of infectious diseases. One digital surveillance that has been used successfully, both globally and in Africa is HealthMap [11]. Health organisations such as World Health Organisation (WHO) rely on systems such as a HealthMap to detect epidemics like the 2014 West African Ebola Outbreak. The strength of HealthMap as an open-source automated disease location detection tool is based on its capability to pool huge, diverse and unstructured Internet data, and extract useful information for users of public health [12]. The system collects alerts daily, categorises them based on the disease and the location, saves them in a database, and then visualises them to the user [11].
In 2021, the WHO launched the Data, Data Analytics and Delivery for Impact in Focus report, to provide an overview of the strategic direction and progress of the WHO Division of Data, Analytics and Delivery for Impact, created as part of Dr. Tedros’ transformation agenda to “address data gaps, focus on results and deliver impact”. The report is a forward-facing tool to support strengthening country health information systems, delivering measurable impact, making data available as a public good and for translating to policy. A SCORE (survey, count, optimize, review and enable) technical package was included to identify gaps and provide necessary tools for countries to address them. WHO completed the first global assessment of countries health information system capacity in 133 countries and the results were reported by region in the Data, Analytics and Delivery for Impact in Focus report, 2022 [13].
Figure 3: SCORE for Health Data Technical Package

Source: WHO (Data, Analytics and Delivery for Impact in Focus 2022)
Figure 4: Percentage distribution of countries by SCORE capacity level, WHO African Region

Source: WHO (Data, Analytics and Delivery for Impact in Focus 2022)
In April, 2023, WHO launched the Health Inequality Data Repository, which contains datasets of disaggregated data, including diverse topics and dimensions of inequality, obtained through publicly available data sources [14].
Furthermore, many African countries have developed national health strategies that prioritize the collection and use of healthcare data. For example, Nigeria has launched a National Health Information System Strategic Plan that aims to improve the quality and availability of healthcare data in the country. Also, some African countries have made significant progress in the use of Electronic Health Records (EHRs). EHRs can improve the quality and accessibility of health data and can help healthcare providers to make better decisions. National eHealth/mhealth strategies have been launched in Ghana in 2010 and 2014 in Malawi and Ethiopia. In countries like Kenya (M-Tiba), South Africa (Hello Doctor), Nigeria (FD Detector) and many others, mobile health (mHealth) technologies are being used to collect and manage health data. mHealth technologies, such as mobile phones and tablets, can help to improve data collection and analysis and can also help to improve healthcare delivery. Even though sophisticated data collection and analysis equipment may not be in place in many parts of Africa to provide world-class healthcare, increased use of social networks (Facebook, Twitter, WhatsApp, etc.), mobile devices and the internet in Africa is making possible the generation of data that can be used for disease surveillance [11]. There is an emerging area in the field of public health called digital epidemiology, which deals with how data can be used to detect, understand, and tackle public health challenges [15]. Several African countries have also made progress in the development of Health Information Systems (HISs). HISs can help to improve the collection, management, and analysis of health data and can help to improve healthcare delivery. A notable development is the introduction of the District Health Information System (DHIS), which is an open-source software platform for reporting, quality checks, visualisation, analysis and dissemination of data for all health programmes. From 2010 onwards, an increasing number of countries began to introduce the web-based DHIS2 platform, and today 70% of countries in Africa are using this electronic platform [15].
Fig 5: DHIS2 in action map
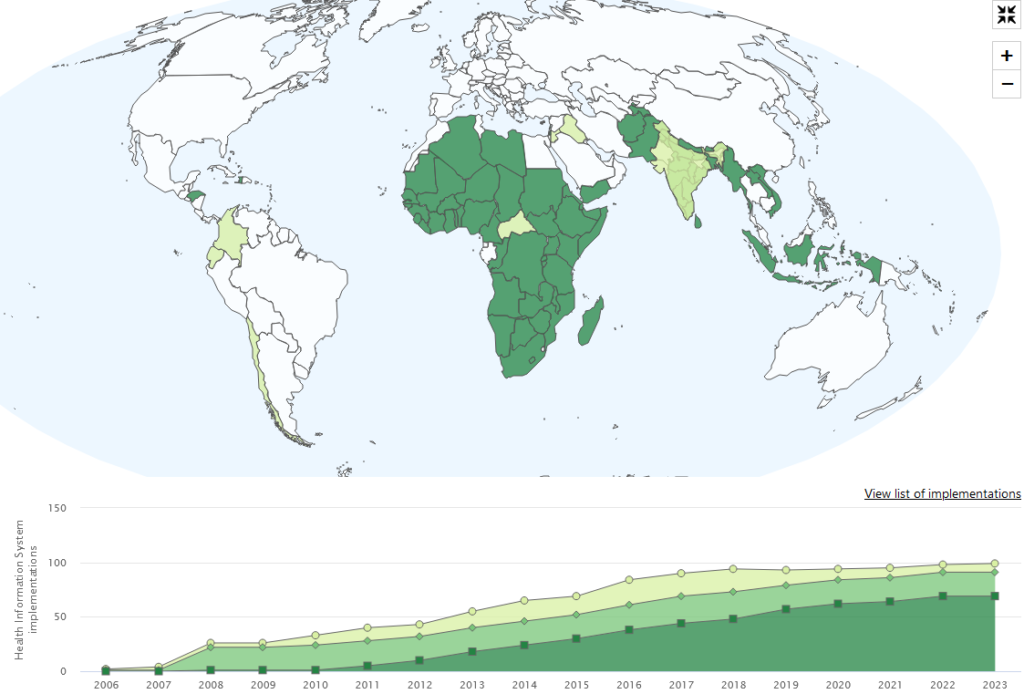
Legend

Call to Action
Addressing these challenges can be done through the development of integrated, and innovative approaches to strengthen health system data quality, analysis, use and access. These approaches include common data standards, digital platforms such as electronic health records and mobile health analytics, real-time data access, as well as multi partner approach.
African countries need to invest in data collection systems to improve the quality and reliability of health data. First, there is a need to invest in healthcare infrastructure, including technology and equipment, to improve data collection and analysis. Governments need to make resources available to meet commitments to providing quality and affordable health care for all through mobilising domestic resources, setting standard data indicators (for collection, analysis and reporting) and strengthening national statistics bodies. Another critical step is to standardize healthcare data collection methods and systems across the continent. This will make it easier to compare and analyze data across different countries and regions. Additionally, African countries should develop the capacity of healthcare professionals in data collection and analysis. This includes training healthcare professionals in data management, analysis, and reporting. Data actors including data managers, statisticians and data analysts need to be involved at every stage, i.e. mapping out the problems, providing solutions and designing research methodologies and “the figuring out how” for collecting, analysing and disseminating data [6]. Finally, there is a need to strengthen collaboration between different stakeholders, including governments, international organizations, and healthcare practitioners, to ensure that healthcare data are accessible and usable.
Conclusion
Despite the prevailing challenges and limitations in Africa, there is evidence that data has the capacity to transform the healthcare system in Africa. Preliminary application in the public health system, especially when epidemics happen has proven evidence of its potential benefits in the African healthcare system. However, in order to make data gains sustainable, there is a need for stakeholders in the African health industry to put in place a roadmap so that data from diverse data sources can be enabled, mined, and transformed into useful actionable knowledge and policy for the benefit of the community. Country ownership is paramount, including the need to prioritise a data-centric approach to quality health care delivery, including the required capacity empowerment to achieve this. Data applications in healthcare are still in its infancy in Africa, thus, reporting success stories of its application can help fast-track its adoption on the continent [11]. African government must also prioritize health, ensuring sustainable funding for health system strengthening, establishing robust health information systems and achieving universal health coverage, in line with quality of health care indicators for meeting the health needs of the vast population, especially those in underserved regions. Targets set through the Abuja declaration and other financing metrics are useful, however, there is need to go beyond ticking the funding box, and ensuring true impact is achieved.

