Author: Hafeez Hamza
World TB Day served as a vital moment to reflect on both the challenges and progress made in the fight against tuberculosis (TB) across Africa. Despite considerable progress, TB remains one of the most devastating infectious diseases on the continent, where high burdens, funding gaps, and socio-economic determinants complicate the fight against this ancient scourge. We examine Africa’s TB landscape, drawing on recent studies and policy reports, and discuss how renewed focus, innovative strategies, and robust investments are essential to achieving TB control and ultimately ending TB as a public health threat.
A Persistent Burden in Africa
TB continues to be a major public health challenge in Africa. Over 95% of TB deaths occur in low and middle-income countries 9. Sub-Saharan Africa (SSA) is among the regions that are highly vulnerable to TB, the continent is home to 17 of the 30 countries with the highest TB burden globally, reporting millions of new cases and hundreds of thousands of deaths every year 2,4. The African region is especially hard hit by TB among children and adolescents; for instance, it was reported that in 2022 approximately 322,000 children and young adolescents fell ill with TB – a figure that represents nearly a third of all childhood TB cases worldwide 2. Such figures underscore the critical need for age-specific interventions and child-friendly diagnostic services.
Over 95% of TB deaths occur in low and middle-income countries
While global progress against TB has yielded reductions in incidence and mortality, progress in Africa remains uneven. Recent analyses indicate that the decline in TB incidence rates and mortality in Africa has not matched the pace observed in other regions, partly due to diagnostic challenges, delayed treatment initiation, and inadequate health system capacities 5. Moreover, the emergence and spread of drug-resistant TB (DR-TB) further complicates the situation, particularly in settings with limited resources.
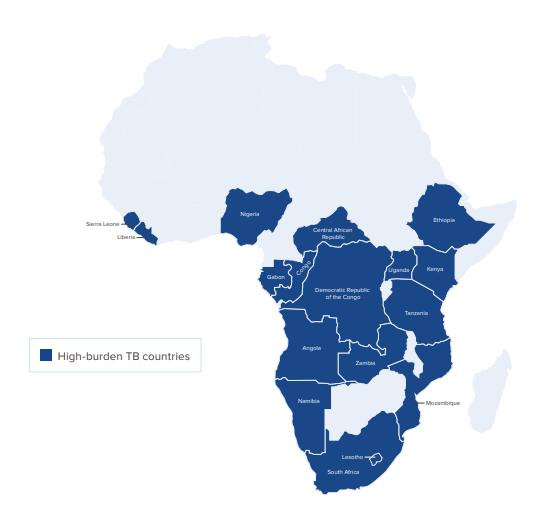
Figure 1 – African countries with the highest burden of TB. Source: EGPAF
Economic and Social Determinants
The TB epidemic in Africa is not only a medical challenge but also a social and economic one. Socio-economic factors, including poverty, malnutrition, and overcrowded living conditions, contribute significantly to the risk of TB infection and progression to active disease 7. Research has consistently shown that TB disproportionately affects the poorest and most vulnerable populations – those who often face the dual burden of disease and financial hardship due to treatment costs and loss of income 2,7.
A scoping review of socio-economic drivers of DR-TB in Africa identified key factors such as substance abuse, stigma, job loss, and the high costs associated with prolonged treatment regimens 7. These factors lead to delayed diagnosis and treatment, and in many cases, poorer treatment outcomes. Addressing these socio-economic determinants is as important as improving medical interventions because they are central to reducing transmission and improving the quality of life of TB patients.
Investing in TB Control: Challenges and Opportunities
Investment in TB control is vital, yet funding gaps persist. Recent data indicate that the African region required at least US $1.3 billion for TB prevention and treatment in 2022, but domestic contributions and international aid together fell short by almost half of this amount 2. Limited resources mean that many TB programs struggle to provide comprehensive diagnostic services, effective treatment, and proper support for patients.
The African region required at least US $1.3 billion for TB prevention and treatment in 2022
Innovative financing mechanisms and stronger domestic commitment are needed to bridge this funding gap. Several international strategies, including the End TB Strategy and the Global Plan to End TB, have underscored the importance of increasing investments to achieve ambitious targets such as a 90% reduction in TB incidence by 2030 8. Recent studies have also demonstrated that every $1 invested in TB control yields significant economic returns – up to $39 in health and economic benefits – further underscoring the potential of well-funded TB programs to boost broader economic growth 2.
Health System Productivity and Efficiency
Improving the productivity and efficiency of TB programs is another critical strategy. Research on health system productivity in sub-Saharan Africa highlights that while technological advancements have been the primary driver of productivity improvements, there remains a significant need to enhance technical efficiency through better resource allocation, capacity building, and improved governance 6. Strengthening the technical efficiency of TB programs not only improves treatment outcomes but also maximizes the impact of available funds, ensuring that investments yield the greatest possible returns in reducing TB burden.
Integration of TB services into broader health systems, especially under universal health insurance schemes, is vital. Such integration can improve access to quality care, reduce treatment delays, and help ensure that TB services reach those most in need. By fostering strong partnerships among governments, international organisations, and civil society, Africa can develop resilient TB programs that are better prepared to handle both current and emerging challenges.
Every $1 invested in TB control yields significant economic returns – up to $39 in health and economic benefits
Innovative Strategies for the Future
Africa’s battle against TB calls for innovative strategies that go beyond conventional approaches. Given the unique challenges on the continent, tailored interventions that address both medical and socio-economic factors are essential. This includes:
- Enhancing Early Diagnosis and Child-Friendly Services: Scaling up access to rapid and accurate diagnostic tools, especially those adapted for children and adolescents, can significantly reduce the delay in treatment initiation and lower transmission rates 2,5.
- Integrating Social Support with Medical Care: Providing social protection measures, such as nutritional support and financial assistance, can help alleviate the economic burden on TB patients. Such integrated approaches have the potential to improve adherence to treatment and reduce default rates, particularly among economically vulnerable groups 7.
- Strengthening Health System Governance: Improving resource management and governance is crucial for enhancing the technical efficiency of TB programs. Investments in capacity building, better training of health professionals, and effective coordination mechanisms are needed to ensure that available resources are used optimally 6.
- Fostering Research and Innovation: Continuous investment in research is critical for the development of new TB vaccines, diagnostic tools, and treatment regimens. The gap in funding for TB research, particularly for vaccine development, remains a barrier to long-term control and eventual eradication of TB 2.
The Imperative of Collective Action
The fight against TB in Africa requires coordinated global and local action. World TB Day serves as a reminder that despite significant strides in reducing TB incidence and mortality, much work remains. Governments, international agencies, and community organisations must work together to mobilise the necessary resources and implement comprehensive strategies that address the full spectrum of challenges posed by TB.
The End TB Strategy sets forth ambitious targets that call for a dramatic reduction in TB cases and deaths. Achieving these targets in Africa will depend not only on scaling up investments and improving service delivery but also on addressing the socio-economic determinants that fuel the TB epidemic. By placing patients and communities at the heart of TB control efforts, Africa can build a more equitable and effective response that not only saves lives but also fosters broader economic and social development.
Conclusion
It is time for Africa to renew its commitment to ending TB. The challenge is formidable: high incidence rates, persistent funding gaps, socio-economic barriers, and the threat of drug-resistant TB all require a multifaceted response. However, with strategic investments, improved health system efficiency, and innovative interventions that are tailored to the unique needs of African populations, there is hope. Africa has the opportunity to transform its TB control efforts into a model for comprehensive, patient-centred care that addresses both medical and social determinants of health.
The journey toward a TB-free Africa is a long one, but each step forward – every dollar invested, every patient treated, every community empowered – brings the continent closer to that goal. In commemoration of World TB Day, let us honour the progress made so far and commit to the decisive action needed to end TB once and for all.
References
- WHO Regional Office for Africa. Rate of TB diagnosis, treatment in Africa increasing. Available from – https://www.afro.who.int/news/rate-tb-diagnosis-treatment-africa-increasing#:~:text=Although%20the%20case%20detection%20rate,WHO)%20Global%20Tuberculosis%20Report%202023. .
- Elizabeth Glaser Pediatric AIDS Foundation. Investing in Tuberculosis Control in Africa. EGPAF. Available from – https://pedaids.org/wp-content/uploads/2024/08/0305-PPA-2024-Brief-TB-Investing-EN-Digital-Final.pdf
- GAVI,The Vaccine Alliance. TB in Africa global report shows successes, but Nigeria and DRC remain important hotspots. Available from – https://www.gavi.org/vaccineswork/tb-africa-global-report-shows-successes-nigeria-and-drc-remain-important-hotspots
- Africa CDC. Tuberculose (TB). Available from – https://africacdc.org/disease/tuberculosis/#:~:text=Tuberculosis%20(TB)%20is%20the%20ninth,Africa%20(2.5%20million%20people)
- WHO Regional Office for Africa. Tuberculose (TB). Available from – https://www.afro.who.int/health-topics/tuberculosis-tb#:~:text=Globally%2C%20TB%20incidence%20has%20fallen,of%20incidence%20compared%20to%202015.
- Atake, EH. Health system productivity in sub-Saharan Africa: tuberculosis control in high burden countries. Cost Eff Resour Alloc 21, 90 (2023) https://doi.org/10.1186/s12962-023-00485-1
- Cannon, LA.L., Oladimeji, K.E. & Goon, D.T. Socio-economic drivers of drug-resistant tuberculosis in Africa: a scoping review. BMC Public Health 21, 488 (2021). https://doi.org/10.1186/s12889-021-10267-0
- World Health Organization. THE END TB STRATEGY. Available from – https://iris.who.int/bitstream/handle/10665/331326/WHO-HTM-TB-2015.19-eng.pdf?sequence=1
- World Health Organization. Tuberculosis. Available from – http://www.tbonline.info/posts/2018/1/16/tb-2018/